Select the ONE answer that is BEST in each case.
A 42-year-old man of Eastern European Jewish descent develops aseptic necrosis of the femoralhead. The other femur shows evidence of osteopenia, and there is diffuse osteopenia of the spine with some collapse. Review of medical records reveals he has had splenomegaly and mild pancytopenia for years. A bone marrow examination is abnormal for infiltration with lipid-laden macrophages called “Gaucher cells.” Which of the following is the most likely mechanism for this condition?
Each syndrome in the lysosomal storage diseases is caused by a mutation-produced deficiency in the activity of a lysosomal enzyme. For example, Tay-Sachs disease is caused by a deficiency of hexosaminidase A, resulting in accumulation of GM2 ganglioside. Gaucher’s disease is caused by a deficiency of beta-glucocerebrosidase, resulting in an accumulation of glucosylceramide. It has several forms and, as in this case, is most common in Ashkenazi (Eastern European) Jews. Type I Gaucher’s disease, as described in this case, is the most common type. Severe bone disease and hepatosplenomegaly is characteristic. Lipid-laden macrophages (Gaucher cells) are found in the bone marrow.
A 26-year-old woman develops a red rash over her cheeks and pain, and swelling in both wrists as well as several small joints in her hands. The rash gets worse on sun exposure and involves her cheeks, nose, ears, and chin. Medical evaluation reveals oral ulceration and 3+ proteinuria. Which of the following is the most specific test for diagnosis of this condition?
Anti-Sm detects a protein complexed to six species of small nuclear ribonucleic acid (RNA). It is believed to be very specific for SLE. However, only 30% of patients have a positive test. In the case presented, there are enough clinical criteria (four) to confirm the diagnosis of SLE with 98% specificity and 97% sensitivity.
An 18-year-old man has had fever for several weeks. The fever occurs on an almost daily basis and is associated with an evanescent salmon-colored truncal rash. He has diffuse arthralgias, and an extensive investigation for infections and malignancy is negative. Which of the following is diagnostic of this condition?
Still’s disease (juvenile RA) in an adult may present as fever of unknown origin. Unfortunately, RF is often negative, and a response to NSAIDs along with exclusion of other diseases confirms the diagnosis.
A 32-year-old woman develops symptoms secondary to a dry mouth and dry eyes. She has enlarged salivary glands. Studies for autoantibodies to Ro (SS-A) are positive. A salivary gland biopsy reveals lymphocytic infiltration. Which of the following is the most likely diagnosis?
The sicca syndrome is a recognized feature of Sjögren’s syndrome. It can be primary or secondary to other autoimmune disorders such as RA, SLE, scleroderma, or vasculitis. Primary Sjögren’s syndrome is most common in middle-aged women; sicca symptoms can also occur as a complication of HIV infection or in sarcoidosis. Sjögren’s syndrome is more likely to have positive serology, while the serology in sarcoid or HIV is negative. Both HIV and Sjögren can have lymphocytic infiltration, but in HIV it is predominantly by CD8 + lymphocytes, whereas in Sjögren’s syndrome, the infiltration is by CD4 + lymphocytes. In sarcoidosis, biopsy reveals granulomas.
A young woman presents with a facial rash, arthralgias, and fatigue. The rash on her face is erythematous and raised, her heart and lungs are normal, and wrists are swollen and tender on palpation. She has mild thrombocytopenia (90,000/mL). Which of the following is the most appropriate initial autoantibody test?
ANA is the most important diagnostic autoantibodies in patients being evaluated for SLE. It is rare to have ANA negative SLE. The other antibodies can occur in SLE but not as sensitive for the diagnosis as ANA. AntidsDNA and anti-SM are specific for SLE but not sensitive.
Advertisement
A 39-year-old woman complains of developing painful pale fingers on cold exposure for the past 5 years. Recently, she has noticed swollen fingers and tight skin, which limit flexion and extension. She also has new abdominal symptoms that are bothersome. On examination, the skin on the fingers is smooth and shiny with associated edema. The rest of the examination is normal. Which part of the gastrointestinal (GI) tract is most frequently involved in this condition?
This patient has scleroderma and esophageal symptoms are present in more than 50% of patients. They are due to the reduced tone of the gastroesophageal sphincter and dilation of the distal esophagus. Gastric and small intestinal motility problems can also occur. Vascular ectasia in the GI tract can result in bleeding.
A 57-year-old woman is complaining of frequent headaches and scalp tenderness. She also has arthralgias, fatigue, and discomfort in her jaw when she chews. On examination, her head and neck is normal, but the right temporal artery is tender on palpation. Her erythrocyte sedimentation rate (ESR) is 50 mm/h and hemoglobin 10.5 g/dL. A temporal artery biopsy is obtained for diagnostic confirmation. Which of the following is the most appropriate next step in management?
The response of pain, stiffness, and headaches to 40–60 mg of prednisone is dramatic in giant cell arteritis. The duration of treatment is not known but most patients require treatment for more than 2 years. ESR is used to monitor response to therapy. Patients need treatment and evaluation for the complications of long-term steroid use such as osteoporosis and diabetes.
A 57-year-old man has pain in his left hand and right knee, which is interfering with his work. The pain came on gradually, first in his hand 6 months ago and now in his knee. It is usually fine when he wakes up, but gets worse as the day progresses. There is no history of any trauma, and he is otherwise well. Taking over-the-counter NSAIDs usually relieves the pain. On examination, there is bony soft tissue swelling of his second and third distal interphalangeal (DIP) joints in the left hand and crepitus over the right knee with flexion. There is no erythema or joint effusion. Which of the following is the initial change noticed in the pathogenesis of osteoarthritis?
It is most likely that the primary change in osteoarthritis occurs in the cartilage. It is possible that there is a disruption of the collagen network of the cartilage, specifically a disruption of the “glue” holding together adjacent fibers.
A 22-year-old woman develops color change in her fingers with cold exposure. The fingers turn white, then blue, and finally red. Which of the following statements regarding this condition is incorrect?
Raynaud’s phenomenon may lead to gangrene of the fingers. It can be primary (Raynaud’s disease) or secondary to other diseases, especially scleroderma, in which it can be the presenting symptom. In women, the primary form is common (over 50%), and the phenomenon is generally much more frequent in women. Digital infarction is much more common in relationship to scleroderma than it is in primary Raynaud’s disease.
A 63-year-old man develops pain and swelling in his knee. It appears warm, red, and swollen with decreased range of movement. A diagnostic aspiration is performed. Which of the following will most likely distinguish pseudogout from gout?
Pseudogout (calcium pyrophosphate crystals—CPPD) is distinguishable from gout by positive birefringent crystals. CPPD are short, blunt rhomboids, and urate crystals (seen in gout) are needle-shaped with negative birefringence.
Advertisement
A 54-year-old woman with rheumatoid arthritis (RA) presents with fatigue and low white count (white blood cells [WBC] 2500/mL) on routine blood work. She has no active joint symptoms and her RA is controlled on lowdose methotrexate and NSAIDs. On examination, she has chronic joint deformities of her hands and a palpable spleen, which is a new finding. Which of the following is the most likely diagnosis for her low white count?
The triad of chronic RA, splenomegaly, and neutropenia is called Felty’s syndrome. It is associated with high titers of RF and extraarticular disease. The increased susceptibility to infections is secondary to both decreased neutrophil number and function. Felty’s syndrome is rare in African Americans.
A 74-year-old woman has pain in her left hand and right knee, which started months ago, and is now interfering with her activities. The pain gets worse as the day progresses. There is no history of any trauma, and she is otherwise well. Taking over-the-counter acetaminophen usually relieves the pain. On examination, there is bony soft tissue swelling of her second and third DIP joints in the left hand and crepitus over the right knee with flexion. There is no erythema or joint effusion. Which of the following is the most likely explanation for the joint pain of osteoarthritis?
Osteophytes can cause pain by stretching periosteal nerve endings. Synovial inflammation is frequently seen in osteoarthritis, but not in ligament inflammation. Microfractures, but not macrofractures, commonly cause pain. Muscle spasm can be an important factor in the joint pain.
A 10-year-old child has recurrent signs and symptoms of palpable purpura on the buttocks, arthralgias, colicky abdominal pain, diarrhea, and microscopic hematuria. Which of the following is the most likely diagnosis?
The child most likely has Henoch-Schönlein purpura, an immune complex vasculitis affecting the skin, GI tract, and renal glomeruli. Inciting antigens include upper respiratory tract infections, drugs, foods, and insect bites.
A 75-year-old woman has abrupt onset of soreness, and severe stiffness of the shoulders and upper thighs with low grade fever. Physical examination is entirely normal, but ESR is over 100 mm/h. Which of the following is the most likely diagnosis?
This patient has PMR. Proximal arm and hip muscle/joint discomfort is the hallmark of this disorder. Difficulty in getting out of bed or rising from a chair may suggest polymyositis, but the muscles are normal when muscle strength is assessed. In general, PMR causes painful muscles, not weak muscles. However, pain may lead to profound disuse atrophy and apparent muscle weakness. In these cases, normal CK and nonspecific muscle biopsy still allow accurate differentiation from polymyositis.
A 63-year-old man presents with weakness and hemoptysis, but no fever, cough, or sputum. He has a 60-pack-per-year history of smoking. The chest x-ray (CXR) reveals a lung mass with mediastinal widening. On examination, there is a blue purple discoloration of the upper eyelids and erythema on his knuckles. He has proximal muscle weakness rated 4+/5, normal reflexes, and sensation. Which of the following is the most likely diagnosis for his muscle weakness?
This man has dermatomyositis, a paraneoplastic phenomenon of many cancers. The most common tumors associated with DM have been bronchogenic carcinomas, ovarian cancers, breast cancers, and melanoma but many others have occurred. The malignancy may antedate or postdate the myositis. Older age makes malignancy more likely. The extent of the workup for malignancy, if DM is the presentation, depends on clinical circumstances, but history and physical examination, not x-rays, are the cornerstones of evaluation.
Advertisement
A 27-year-old man has a history of low back pain and stiffness. After several months of mild symptoms, he notes more severe stiffness at night and hip pain. On physical examination, there is paravertebral muscle tenderness and limited flexion of the lumbar spine. X-ray of the lumbar spine shows sacroiliitis. In addition to recommending physiotherapy and exercise, which of the following is the most appropriate next step in management?
All NSAIDs are probably equally effective in the treatment of this man’s ankylosing spondylitis. Options include indomethacin or naproxen, but not phenylbutazone since it can cause aplastic anemia. Exercise and maintaining proper posture are very important.
A 24-year-old woman notices pain in her left arm, made worse with use. She also has fatigue, fever, night sweats, and arthralgias. On examination, there are no palpable lymph nodes, and the joints and muscle strength are normal. The left radial pulse is absent, and there is a bruit over the left subclavian and common carotid arteries. Preliminary laboratory investigations reveal an elevated ESR and mild anemia. Which of the following vascular findings is most likely to be found in her?
High pressure in the legs and low pressure in the arms characterize Takayasu’s syndrome. Clinical manifestations include easy fatigability of the arms and atrophy of the soft tissues of the face. The course is variable, and spontaneous remissions can occur. The disease predominantly affects young women.
Figure shows an x-ray of a 40-year-old Caucasian man with symptoms of sinusitis and an incidental finding in the skull. Which of the following is the most likely diagnosis?
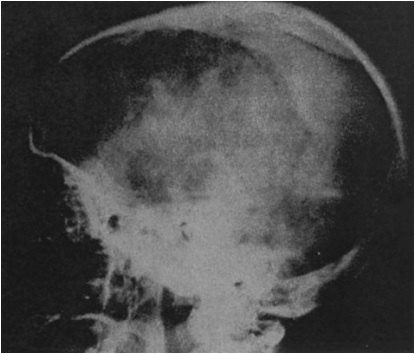
This is a rarefied area involving the frontal and parietal bones, and it is an early stage of Paget’s disease in which calvarial thickening and foci or radiopacity are not present within the radiolucent area. At this stage of the disease, a cross-section through the margin of the lesion reveals a compact inner and outer table in the normal portion, whereas the diploe widens and extends to the outer and inner surfaces of the calvarium without a change in the calvarial thickness in the lesion.
A 34-year-old woman develops a red rash over her cheeks, frequent oral ulcers, and pain and swelling in both wrists as well as in several small joints in her hands. Medical evaluation reveals a positive ANA, and 3+ proteinuria. Which of the following organ involvement will cause the most symptoms during the course of this disease?
About 95% of patients will develop musculoskeletal symptoms during the course of SLE. Arthralgias and myalgias predominate, but arthritis, hand deformities, myopathy, and avascular necrosis of bone also occur. About 85% of patients will have hematologic disease and 80% will have skin manifestations.
. A 29-year-old woman develops painful swelling of both hands. She is also very stiff in the morning. Physical examination reveals involvement of the proximal interphalangeal joints and metacarpophalangeal (MCP) joints. Her RF is positive and ANA is negative. Which of the following medications is most likely to improve her joint pain symptoms?
This patient has RA and aspirin or other nonsteroidal agents are effective medications for relieving the signs and symptoms of disease. They do little to modify the course of the disease, however. The new generation of NSAIDs that are more specific inhibitors of cyclooxygenase 2 cause less GI toxicity. Glucocorticoids are very powerful at suppressing signs and symptoms of disease and may alter disease progression. Methotrexate is an important disease modifying drug (DMRD) used to prevent joint destruction. Gold and antimalarials were important DMRDs in the past before the use of methotrexate and newer “biological” agents.
Share your Results:
See all quizzes of the Muscles and joints at here:
Part 1 | Part 2 | Part 3 | Part 4|
| 1. A 42-year-old man of Eastern European Jewish descent develops aseptic necrosis of the femoralhead. The other femur shows evidence of osteopenia, and there is diffuse osteopenia of the spine with some collapse. Review of medical records reveals he has had splenomegaly and mild pancytopenia for years. A bone marrow examination is abnormal for infiltration with lipid-laden macrophages called “Gaucher cells.” Which of the following is the most likely mechanism for this condition?
(A) insulin deficiency (B) abnormal elastic tissue (C) excess iron in tissue (D) homocystinuria (E) abnormal lysosomal enzymes |
| 2. A 26-year-old woman develops a red rash over her cheeks and pain, and swelling in both wrists as well as several small joints in her hands. The rash gets worse on sun exposure and involves her cheeks, nose, ears, and chin. Medical evaluation reveals oral ulceration and 3+ proteinuria. Which of the following is the most specific test for diagnosis of this condition?
(A) lupus erythematosus (LE) cells (B) antinuclear antibody (ANA) (C) anti-Sm antibody (D) anti-Ro antibody (E) antiphospholipid antibody |
| 3. An 18-year-old man has had fever for several weeks. The fever occurs on an almost daily basis and is associated with an evanescent salmon-colored truncal rash. He has diffuse arthralgias, and an extensive investigation for infections and malignancy is negative. Which of the following is diagnostic of this condition?
(A) high-titer rheumatoid factor (RF) (B) positive ANA (C) response to steroid therapy (D) response to nonsteroidalantiinflammatory drug (NSAID) therapy (E) lymph node biopsy |
| 4. A 32-year-old woman develops symptoms secondary to a dry mouth and dry eyes. She has enlarged salivary glands. Studies for autoantibodies to Ro (SS-A) are positive. A salivary gland biopsy reveals lymphocytic infiltration. Which of the following is the most likely diagnosis?
(A) sarcoidosis (B) primary Sjögren’s syndrome (C) human immunodeficiency virus (HIV) infection (D) lymphoma (E) amyloidosis |
| 5. A young woman presents with a facial rash, arthralgias, and fatigue. The rash on her face is erythematous and raised, her heart and lungs are normal, and wrists are swollen and tender on palpation. She has mild thrombocytopenia (90,000/mL). Which of the following is the most appropriate initial autoantibody test?
(A) anti-double-stranded (ds) deoxyribonucleic acid (DNA) (B) anti-Sm (C) anti-Ro or La (D) ANA (E) antiphospholipid antibodies (lupus anticoagulant) |
| 6. A 39-year-old woman complains of developing painful pale fingers on cold exposure for the past 5 years. Recently, she has noticed swollen fingers and tight skin, which limit flexion and extension. She also has new abdominal symptoms that are bothersome. On examination, the skin on the fingers is smooth and shiny with associated edema. The rest of the examination is normal. Which part of the gastrointestinal
(GI) tract is most frequently involved in this condition? (A) esophagus (B) stomach (C) duodenum (D) ileum (E) colon |
| 7. A 57-year-old woman is complaining of frequent headaches and scalp tenderness. She also has arthralgias, fatigue, and discomfort in her jaw when she chews. On examination, her head and neck is normal, but the right temporal artery is tender on palpation. Her erythrocyte sedimentation rate (ESR) is 50 mm/h and hemoglobin 10.5 g/dL. A temporal artery biopsy is obtained for diagnostic confirmation. Which of the following is the most appropriate next step in management?
(A) intravenous high-dose steroids (B) acetylsalicylic acid (C) indomethacin (D) low-dose (prednisone 40 mg/day) steroids by mouth (E) topical steroid creams |
| 8. A 57-year-old man has pain in his left hand and right knee, which is interfering with his work. The pain came on gradually, first in his hand 6 months ago and now in his knee. It is usually fine when he wakes up, but gets worse as the day progresses. There is no history of any trauma, and he is otherwise well. Taking over-the-counter NSAIDs usually relieves the pain. On examination, there is bony soft tissue swelling of his second and third distal interphalangeal (DIP) joints in the left hand and crepitus over the right knee with flexion. There is no erythema or joint effusion. Which of the following is the initial change noticed in the pathogenesis of osteoarthritis?
(A) abnormal chondrocyte function (B) a defect in the extracellular matrix of cartilage (C) inflammatory changes in subchondral bone (D) ligament inflammation (E) synovial inflammation |
| 9. A 22-year-old woman develops color change in her fingers with cold exposure. The fingers turn white, then blue, and finally red. Which of the following statements regarding this condition is incorrect?
(A) may lead to gangrene of the fingers (B) may precede the onset of scleroderma (C) symptoms can be brought on by vibration or stress (D) pallor (white color) associated with coldness and numbness while rubor (red color) associated with pain and tingling (E) affects the sexes equally |
| 10. A 63-year-old man develops pain and swelling in his knee. It appears warm, red, and swollen with decreased range of movement. A diagnostic aspiration is performed. Which of the following will most likely distinguish pseudogout from gout?
(A) positive birefringent crystals (B) acute onset (C) involvement of single joints (D) involvement of large joints (E) association with diabetes |
| 11. A 54-year-old woman with rheumatoid arthritis (RA) presents with fatigue and low white count (white blood cells [WBC] 2500/mL) on routine blood work. She has no active joint symptoms and her RA is controlled on lowdose methotrexate and NSAIDs. On examination, she has chronic joint deformities of her hands and a palpable spleen, which is a new finding. Which of the following is the most likely diagnosis for her low white count?
(A) methotrexate therapy (B) rheumatoid nodules disrupting bone marrow architecture (C) Felty’s syndrome (D) normal variation (E) myelofibrosis |
| 12. A 74-year-old woman has pain in her left hand and right knee, which started months ago, and is now interfering with her activities. The pain gets worse as the day progresses. There is no history of any trauma, and she is otherwise well. Taking over-the-counter acetaminophen usually relieves the pain. On examination, there is bony soft tissue swelling of her second and third DIP joints in the left hand and crepitus over the right knee with flexion. There is no erythema or joint effusion. Which of the following is the most likely explanation for the joint pain of osteoarthritis?
(A) synovial inflammation is not the cause (B) ligament inflammation is a common cause (C) clinically visible (via plain x-ray) fractures are a common cause of pain (D) osteophytes can cause pain (E) muscles are not involved |
| 13. A 10-year-old child has recurrent signs and symptoms of palpable purpura on the buttocks, arthralgias, colicky abdominal pain, diarrhea, and microscopic hematuria. Which of the following is the most likely diagnosis?
(A) influenza (B) immune complex vasculitis (C) juvenile RA (D) systemic lupus erythematosus (SLE) (E) Wegener’s granulomatosis |
| 14. A 75-year-old woman has abrupt onset of soreness, and severe stiffness of the shoulders and upper thighs with low grade fever. Physical examination is entirely normal, but ESR is over 100 mm/h. Which of the following is the most likely diagnosis?
(A) dermatomyositis (DM) (B) osteoarthritis (C) polymyalgia rheumatica (PMR) (D) midline granuloma (E) sarcoidosis |
| 15. A 63-year-old man presents with weakness and hemoptysis, but no fever, cough, or sputum. He has a 60-pack-per-year history of smoking. The chest x-ray (CXR) reveals a lung mass with mediastinal widening. On examination, there is a blue purple discoloration of the upper eyelids and erythema on his knuckles. He has proximal muscle weakness rated 4+/5, normal reflexes, and sensation. Which of the following is the most likely diagnosis for his muscle weakness?
(A) SLE (B) scleroderma (C) dermatomyositis (DM) (D) polyarteritis (E) Weber-Christian disease |
| 16. A 27-year-old man has a history of low back pain and stiffness. After several months of mild symptoms, he notes more severe stiffness at night and hip pain. On physical examination, there is paravertebral muscle tenderness and limited flexion of the lumbar spine. X-ray of the lumbar spine shows sacroiliitis. In addition to recommending physiotherapy and exercise, which of the following is the most appropriate next step in management?
(A) NSAID therapy (B) phenylbutazone (C) azathioprine (D) acetaminophen (E) prednisone |
| 17. A 24-year-old woman notices pain in her left arm, made worse with use. She also has fatigue, fever, night sweats, and arthralgias. On examination, there are no palpable lymph nodes, and the joints and muscle strength are normal. The left radial pulse is absent, and there is a bruit over the left subclavian and common carotid arteries. Preliminary laboratory investigations reveal an elevated ESR and mild anemia. Which of the following vascular findings is most likely to be found in her?
(A) high pressure in the legs and low pressure in the arms (B) low pressure in the legs and high pressure in the arms (C) high-pitched diastolic murmur (D) a relentless course to death (E) hypotension |
| 18. Figure 9–1 shows an x-ray of a 40-year-old Caucasian man with symptoms of sinusitis and an incidental finding in the skull. Which of the following is the most likely diagnosis?
(A) normal variant (B) osteomyelitis (C) Paget’s disease (D) hemangioma (E) metastatic disease |
| 19. A 34-year-old woman develops a red rash over her cheeks, frequent oral ulcers, and pain and swelling in both wrists as well as in several small joints in her hands. Medical evaluation reveals a positive ANA, and 3+ proteinuria. Which of the following organ involvement will cause the most symptoms during the course of this disease?
(A) renal pathology (B) cardiopulmonary pathology (C) musculoskeletal pathology (D) thrombotic events (E) skin changes |
| 20. A 29-year-old woman develops painful swelling of both hands. She is also very stiff in the morning. Physical examination reveals involvement of the proximal interphalangeal joints and metacarpophalangeal (MCP) joints. Her RF is positive and ANA is negative. Which of the following medications is most likely to improve her joint pain symptoms?
(A) D-penicillamine (B) an antimalarial (C) methotrexate (D) NSAID or aspirin (E) gold |
